Some more data:
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Health expenditure
- Thread starter Mikefromcork
- Start date
Are we not talking about the greater dependency?
Across the board, does the private health sector have a greater dependency on the public health sector or vice versa?
You are correct. What is not always obvious is that private care in Ireland has a distorting effect. They deliver services which are more profitable and they are not burdened by the fixed-cost, resource-intensive services provided by the HSE. The outsourcing of care, like the NTPF, has massive opportunity costs and negative downstream effects on capital budgets, current expenditure, staff training, and workforce planning. These are easy to miss if the system is viewed transactionally.
Look at the opening hours of private A&Es and the list of things they exclude. This is because the overheads for a full-service A&E are huge. They also deal with a different demographic - you will not find pregnant women, patients with psychiatric issues, homeless people with addiction issues, etc. as they all require significant resources and private hospitals cannot afford to pay for loss leaders, so the HSE takes these on.
Are you saying that if there was no Private Healthcare system there would be less or equal public spending on healthcare?You are correct. What is not always obvious is that private care in Ireland has a distorting effect. They deliver services which are more profitable and they are not burdened by the fixed-cost, resource-intensive services provided by the HSE. The outsourcing of care, like the NTPF, has massive opportunity costs and negative downstream effects on capital budgets, current expenditure, staff training, and workforce planning. These are easy to miss if the system is viewed transactionally.
Look at the opening hours of private A&Es and the list of things they exclude. This is because the overheads for a full-service A&E are huge. They also deal with a different demographic - you will not find pregnant women, patients with psychiatric issues, homeless people with addiction issues, etc. as they all require significant resources and private hospitals cannot afford to pay for loss leaders, so the HSE takes these on.
Unless that is the case it is true to say that the Private Healthcare system subsidises the Public Healthcare system.
The Public System is there for all of the people. If some use private healthcare instead then the burden on the public system is reduced.
Sophrosyne
Registered User
- Messages
- 1,543
That's irrelevant. Even if the private system cherry picks the easier cases it's still taking that workload off the public system.Are we not talking about the greater dependency?
The private system absolutely depends on the public system more.Across the board, does the private health sector have a greater dependency on the public health sector or vice versa?
If I go to the GP and pay for it myself but get a partial reimbursement from my insurance company there is no cost to the State. If I have access free at the point of use GP care through the GMS then there is a cost to the State. The fact that the State already pays the GP's pension, the practice nurse, the practice manager and about €170k a year in wages to the GP is of no consequence. What matters is that if I was getting "Free" GP care the State would be paying the GP somewhere between €68 and €335 additionally per year.
The HF3 category above shows the private household payments not covered by insurance.Agreed @arbitron.
The full economic costs are often missed.
Add to that the subsidization of private operators, such as GPs, Dentists,etc.
The alternative to households making those payments is for the State to make them.
It is.The private income receives by GP's and Dentists isn't included in the healthcare spending figures.
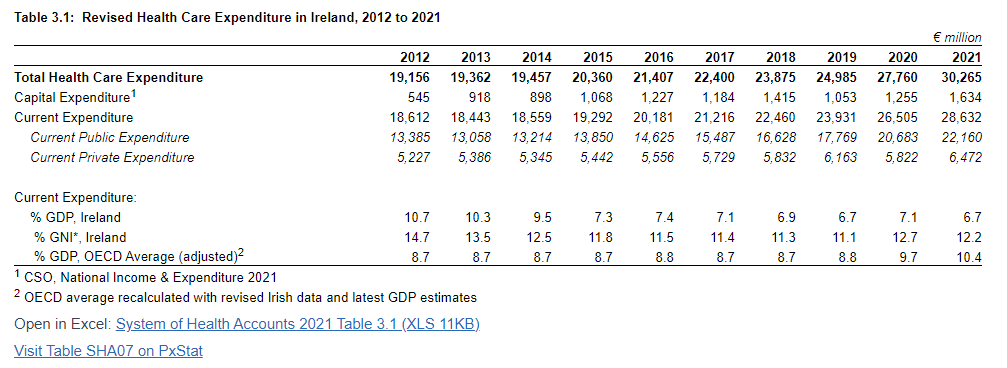
If it is paid by insurers or out of pocket it is included in the CSO SHA data above.
I've edited my post. In the context of the discussion it was very misleading.It is.
If it is paid by insurers or out of pocket it is included in the CSO SHA data above.
The CSO data shows that it is an additional subsidy of the Public System.
Sophrosyne
Registered User
- Messages
- 1,543
The figure you need to look at for Ireland is GNI*, which corrects the distortion of multi-nationals on our GDP.o our healthcare expenditure is less than 2/3rds of the OECD average in GDP terms.......how far below the average should we be, Purple?
Sophrosyne
Registered User
- Messages
- 1,543
Of course, it is relevant.That's irrelevant. Even if the private system cherry picks the easier cases it's still taking that workload off the public system.
The private system absolutely depends on the public system more.
If I go to the GP and pay for it myself but get a partial reimbursement from my insurance company there is no cost to the State. If I have access free at the point of use GP care through the GMS then there is a cost to the State. The fact that the State already pays the GP's pension, the practice nurse, the practice manager and about €170k a year in wages to the GP is of no consequence. What matters is that if I was getting "Free" GP care the State would be paying the GP somewhere between €68 and €335 additionally per year.
Firstly, private health treatment whether provided by a hospital, GP, Dentist, Pharmacy,etc is an additional cost to the individual. Focusing exclusively on exchequer spending does not reflect the total healthcare burden on citizens.
Secondly, while the private sector might provide a small subsidy, it could not by any stretch be said to “prop up” the public sector, when it is “propped up” itself because it does not bear the full economic cost of what it provides.
Mikefromcork
Registered User
- Messages
- 42
Hi AllJust wondering given the cut in health expenditure compared to last year, rising healthcare costs with inflation and the deficit the HSE is running, no new programmes approved.
1 where are the new beds promised going to come from.
2 Surely our health system is going to even get worst this winter?
I am just going back to my initial post.
1) With the increase yesterday will our hospital system get the new beds and 2) will we be in a worse state this year or has there been changes to ensure this won’t happen again.
Best wishes
Mike
Unlikely as the funding does not match the expectation/demand. Extra beds require extra staff and recruitment is very difficult.1) With the increase yesterday will our hospital system get the new beds
Very little is going to change in the coming months - any significant improvements would likely take years.and 2) will we be in a worse state this year or has there been changes to ensure this won’t happen again.
Given the problems with GDP, GNP in Ireland, I use h/care exp per person instead.
It should be lower in Ireland that most EU countries, due to the younger age profile of our population.
It is 6,030 euro in 2022, higher than FR or DE.
It is the highest among the euro countries (excludes LUX).
This is partly caused by high prices here, e.g. GP charges 26 in France.
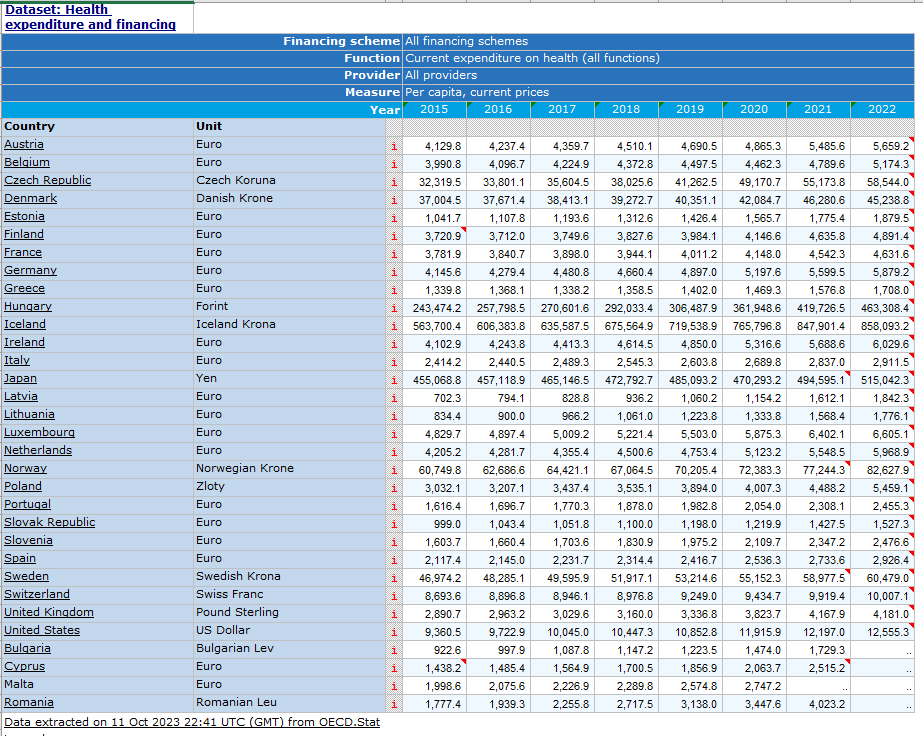
It should be lower in Ireland that most EU countries, due to the younger age profile of our population.
It is 6,030 euro in 2022, higher than FR or DE.
It is the highest among the euro countries (excludes LUX).
This is partly caused by high prices here, e.g. GP charges 26 in France.
Thank you Protocol - that's great data.
I was hoping the ball a little with Purple yesterday - but one serious question - how do we know we are comparing apples with apples?
Take Ireland v France. How is nursing home care treated in these figures in both countries?
I was hoping the ball a little with Purple yesterday - but one serious question - how do we know we are comparing apples with apples?
Take Ireland v France. How is nursing home care treated in these figures in both countries?
It's not relevant in the context of the Government's spend on healthcare. I completely agree that it is relevant in the context of overall spend. That's the point I'm making; private health insurance and out of pocket expenditure is a subsidy of the public system. If the public system was structured and run properly then private citizens would have far fewer out of pocket expenses and there would be far less need for private health insurance.Of course, it is relevant.
Firstly, private health treatment whether provided by a hospital, GP, Dentist, Pharmacy,etc is an additional cost to the individual. Focusing exclusively on exchequer spending does not reflect the total healthcare burden on citizens.
Yes, it is a subsidy rather than a stand alone system. It provides 12-13% of the total healthcare by cost.Secondly, while the private sector might provide a small subsidy, it could not by any stretch be said to “prop up” the public sector, when it is “propped up” itself because it does not bear the full economic cost of what it provides.
Thank you Protocol - that's great data.
I was hoping the ball a little with Purple yesterday - but one serious question - how do we know we are comparing apples with apples?
Take Ireland v France. How is nursing home care treated in these figures in both countries?
I am not an expert in this idea, but here you go:
International Classification of Health Accounts
This section provides some detail on each classification. Details of the current application of the standard in Ireland are available in metadata which is in the System of Health Accounts methodology section, see https://t4.cso.ie/terminalfour/preview/10/en/28336 (methodology).ICHA – HF: Health Care Financing Schemes
Health care financing schemes are structural components of health care financing systems. They are the main types of financing arrangements through which people obtain health services. These include:- Government schemes
- Compulsory contributory health insurance
- Voluntary health insurance
- Other financing arrangements in which participation is voluntary
- Out-of-pocket expenditure by households.
The classification of health care providers (ICHA-HP) classifies all organisations that contribute to the provision of health care goods and services, by arranging country-specific provider units into common, internationally applicable categories. The “principal activity” undertaken is the basic criterion for classifying health care providers. These include:
- Hospitals
- Residential long-term care facilities (e.g. for older people or for people with a disability)
- Ambulatory health care providers (e.g. GPs, dentists)
- Ancillary service providers (e.g. transport, emergency rescue, laboratory services)
- Retailers and other providers of medical goods (e.g. pharmacies)
- Providers of preventive care (e.g. organisation of public health programmes)
- Providers of health care administration and financing
- Other providers (e.g. households, other industries, rest of world)
The functional classification under the SHA is the key classification for defining the boundary of health care. It groups health care services by purpose. The first five categories relate to goods and services consumed by individuals. These categories comprise
- Curative and rehabilitative care – where the principal intent is to:
- Relieve symptoms of illness or injury, to reduce the severity of an illness or injury, or to protect against exacerbation and/or complication of an illness and/or injury that could threaten life or normal functioning; and/or
- To empower persons with health conditions who are experiencing or are likely to experience disability so that they can achieve and maintain optimal functioning, a decent quality of life and inclusion in the community and society.
- Long-term care (health) – which consists of a range of medical and personal care services with the primary goal of alleviating pain and suffering and reducing or managing the deterioration in health status in patients with a degree of long-term dependency. The SHA distinguishes between long-term care with a “health” purpose and long-term care with a “social” purpose. As these elements of long-term care are often delivered in a single package of care, it is difficult to separate them.
- Ancillary services such as laboratory services, imaging services, patient transport and emergency rescue. Data is reported explicitly in this category only when the services are received independently of an overall episode of health care – the majority of these services are recorded as part of curative and rehabilitative or long-term care and are not separately identified.
- Medical goods dispensed to outpatients – by a health care establishment or by a retailer of medical goods. Like ancillary services, those goods consumed as part of other functions are not identified separately.
- Prevention and public health services – such as information, education and counselling programmes, immunisation programmes, screening programmes and disease surveillance.
- Health administration and governance – includes the formulation and administration of government policy; the setting of standards; the regulation, licensing or supervision of producers. These activities are mainly carried out by governments but may also be provided by private bodies such as health insurers and advocacy/representative groups.
I was hoping the ball a little with Purple yesterday - but one serious question - how do we know we are comparing apples with apples?
Take Ireland v France. How is nursing home care treated in these figures in both countries?
I recall reading something about how LT care is captured in the data.
I am trying to find it.
An academic article in 2017:
Another article from 2020:
How does Irish Healthcare Expenditure compare internationally?
The ESRI research report ‘How does Irish Healthcare Expenditure compare internationally?’ examines how Irish Healthcare Expenditure (HCE) compares to expenditure in other countries. Using international OECD data for 2017, this study finds that how Irish HCE compares differs depending on the...
The ESRI research report ‘How does Irish Healthcare Expenditure compare internationally?’ examines how Irish Healthcare Expenditure (HCE) compares to expenditure in other countries. Using international OECD data for 2017, this study finds that how Irish HCE compares differs depending on the expenditure measure used, the service examined and whether the comparison is adjusted for countries’ differing approaches to accounting for Social Care Expenditure.
HCE as a share of national income is a measure that is often used to rank countries’ HCE. However, adjusting for population and relative prices, with the aim of comparing the volume of healthcare consumed per capita, is found to have a considerable impact on rankings of HCE across countries.
Not all countries include the same items in Healthcare Expenditure. Adjusting for countries’ differing accounting methods, by including both HCE and Healthcare-Related Expenditure (HCRE) in international comparison, also changes rankings across countries.
Main findings
The main findings of this study, based on 2017 data and rankings in the EU15, are:
- Irish HCE ranks differently depending on the measure of HCE examined:
- Ireland’s total HCE as a share of national income (1) ranks 1st
- National income measured as modified GNI for Ireland and GDP for other countries
- Ireland’s total HCE per capita with adjustment for relative prices ranks 9th
- Irish public HCE per capita (2) ranks 9th, while private HCE per capita ranks 2nd
- Countries are inconsistent in their accounting for Social Care:
- Ten EU15 countries allocated some Social Care Expenditure in 2017 to Healthcare-Related Expenditure (HCRE), which is not counted in HCE
- The Netherlands assigned 12 per cent and the UK assigned 5 per cent of combined Health and Social Care expenditure to HCRE
- Ireland allocated €4.6 billion in Social Care Expenditures to HCE (22 per cent of Total HCE) and none to HCRE
- Ireland includes over €900 million in payments to family carers in HCE, comprising 4.3 per cent of total Irish HCE, but the Netherlands does not include these payments in HCE
- Ireland includes all expenditure on home care services, group homes in the community for people with disabilities and day services for older people under HCE, while the UK excludes much of this expenditure from HCE
- If Health and Social Care combined are compared, Irish public HCE per capita with adjustment for relative prices ranks 10th in the EU15
The authors advise caution in applying evidence from international databases to interpret relative Healthcare Expenditure or health system performance. Social Care Expenditure accounted for under HCRE should be included in cross-country comparison of healthcare expenditures. The analysis concludes that ambiguity in OECD System of Health Accounts (SHA) guidelines, combined with Irish data challenges, has led to an overestimation of Irish HCE. The Irish approach to SHA accounting for Social Care Expenditure could warrant review, supported by improved data.
Differing rankings for volume and price measures demonstrate that relatively high HCE may indicate, as in the case of Ireland, a relatively high-price, high-wage economy rather than a relatively high volume of services delivered. Differing rankings for public and private expenditures in Ireland suggest that understanding Ireland’s relatively high HCE as a share of national income requires an understanding of Ireland’s private healthcare system.
Although Ireland has apparently high expenditure on home-based care, this reflects payments to family members of people with disabilities and inclusion of some disability residential services under this heading. When professional home care services are compared, Irish per capita HCE is under half the EU15 mean. Similarly, Irish HCE per capita on inpatient care in public and private hospitals is below the EU15 mean.
Dr Maev-Ann Wren, ESRI Senior Research Officer and lead author, said:
“Healthcare expenditure is sometimes understood as expenditure on hospital services, leading to a disconnect between Ireland’s apparently high HCE and over-stressed hospital system. Our findings examining the many categories of Health and Social Care expenditure which Ireland includes in HCE, makes clear that Ireland’s comparative HCE should not be interpreted as a measure of hospital service expenditure.
Understanding Ireland’s apparently relatively high HCE needs to be informed by an understanding that Ireland’s relatively high prices and wages have obscured the continuing relatively low volume of Irish healthcare services delivered. It is against this backdrop that the Irish health authorities, the HSE and the Department of Health, prepared for the pandemic surge, with understandable fear that the public healthcare system might be overwhelmed. We hope that the analysis in this report will contribute to a better understanding of international HCE comparisons to inform the development and strengthening of the Irish healthcare system.”
[1] National income measured as modified GNI for Ireland and GDP for other countries
[2] All per capita findings also include adjustment for relative prices